2024-09-24 12:28:53
Gram-Negative Bacteria majorpublished
Did you know?
Gram-negative bacteria can trigger deadly septic shock by releasing toxins from their outer membrane when they are destroyed.
Gram-negative bacteria are resilient pathogens with antibiotic resistance, causing infections like TIs, sepsis, and pneumonia.
Karen Pendergrass is a microbiome researcher specializing in microbiome-targeted interventions (MBTIs). She systematically analyzes scientific literature to identify microbial patterns, develop hypotheses, and validate interventions. As the founder of the Microbiome Signatures Database, she bridges microbiome research with clinical practice. In 2012, based on her own investigative research, she became the first documented case of FMT for Celiac Disease—four years before the first published case study.
Microbiome Signatures identifies and validates condition-specific microbiome shifts and interventions to accelerate clinical translation. Our multidisciplinary team supports clinicians, researchers, and innovators in turning microbiome science into actionable medicine.
Karen Pendergrass is a microbiome researcher specializing in microbiome-targeted interventions (MBTIs). She systematically analyzes scientific literature to identify microbial patterns, develop hypotheses, and validate interventions. As the founder of the Microbiome Signatures Database, she bridges microbiome research with clinical practice. In 2012, based on her own investigative research, she became the first documented case of FMT for Celiac Disease—four years before the first published case study.
Gram-negative bacteria are a diverse group of microorganisms characterized by their inability to retain the crystal violet stain in the Gram staining method due to their cell wall structure. Unlike Gram-positive bacteria, Gram-negative bacteria have a thin peptidoglycan layer sandwiched between an inner cytoplasmic membrane and an outer membrane containing lipopolysaccharides (LPS). This structural difference contributes to their unique biological behavior and increased antibiotic resistance. [1] Gram-negative bacteria are involved in numerous human diseases, particularly hospital-acquired infections. Their ability to evade the immune system and resist treatment makes them formidable pathogens. Infections caused by Gram-negative bacteria can range from mild to life-threatening, particularly when they lead to sepsis, where the release of endotoxins (LPS) can cause septic shock.
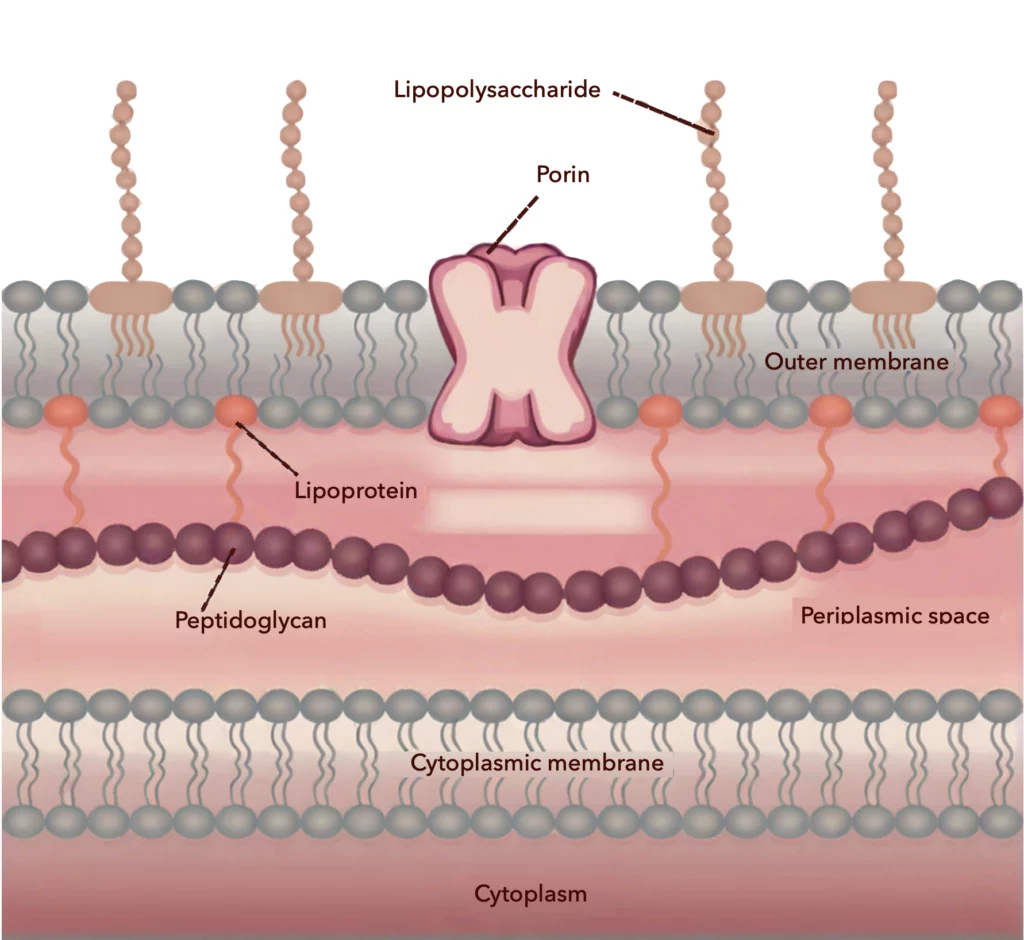
The defining feature of Gram-negative bacteria is their cell envelope, consisting of an inner cytoplasmic membrane, a thin peptidoglycan layer, and an outer membrane. Between the inner and outer membranes, these bacteria have a gel-like periplasmic space, which contains enzymes and proteins vital for nutrient acquisition and antibiotic resistance. The outer membrane is composed of lipopolysaccharides (LPS) on its outer leaflet and phospholipids on the inner leaflet, with porins acting as channels for molecules. The lipid A component of LPS is an endotoxin that can trigger inflammatory responses in humans, leading to septic shock in severe cases. The dual membrane structure of these bacteria not only makes them more resistant to environmental stressors but also to antibiotics, detergents, and lysozymes produced by the host immune system.
Many gram-negative species are significant human pathogens, known for causing respiratory, urinary, gastrointestinal, and bloodstream infections. Their outer membrane is a formidable barrier against antibiotics, making them difficult to treat. The lipopolysaccharides (LPS) in their outer membrane can trigger severe immune responses when they enter the bloodstream, leading to septic shock, which can be fatal if untreated. In addition to their outer membrane, they possess other resistance mechanisms, such as efflux pumps that expel toxic substances (including antibiotics), enzymes in the periplasmic space that degrade or modify antibiotics, and porins that regulate the entry of drugs, often reducing their effectiveness. While several classes of antibiotics, including aminoglycosides, cephalosporins, quinolones, monobactams, and carbapenems, are used to target Gram-negative bacteria, the rising prevalence of multidrug resistance in species like Pseudomonas aeruginosa and Acinetobacter baumannii presents ongoing treatment challenges.
Gram-negative bacteria were historically grouped based on their staining properties, dividing bacteria into Gram-positive (monoderm) and Gram-negative (diderm). While this classification was initially considered to reflect phylogenetic lineages, modern molecular studies have shown that the Gram-negative category is not a monophyletic group. Gram-negative bacteria are divided into various phyla and are further classified based on their cell wall structure and genetic makeup.
Below is a list of some medically relevant Gram-negative bacteria, including the diseases they are known to cause.
| Species | Pathogenic Role |
|---|---|
| Escherichia coli | Causes urinary tract infections (UTIs), gastroenteritis, and neonatal meningitis. |
| Pseudomonas aeruginosa | Causes respiratory infections, wound infections, and sepsis, especially in hospitals. |
| Neisseria gonorrhoeae | Responsible for the sexually transmitted infection gonorrhea. |
| Neisseria meningitidis | Causes bacterial meningitis and septicemia. |
| Klebsiella pneumoniae | Causes pneumonia, bloodstream infections, and UTIs. |
| Haemophilus influenzae | Causes respiratory infections, particularly in children, and meningitis. |
| Legionella pneumophila | Causes Legionnaires’ disease, a severe form of pneumonia. |
| Salmonella enterica | Causes foodborne illnesses, including gastroenteritis and typhoid fever. |
| Helicobacter pylori | Linked to peptic ulcers and gastric cancer. |
| Vibrio cholerae | Causes cholera, a severe diarrheal disease. |
| Acinetobacter baumannii | Causes hospital-acquired infections, including ventilator-associated pneumonia. |
| Shigella dysenteriae | Causes dysentery, leading to severe diarrhea and intestinal inflammation. |
| Yersinia pestis | Responsible for plague, including bubonic and pneumonic forms. |
| Proteus mirabilis | Common cause of UTIs and wound infections. |
| Chlamydia trachomatis | Causes sexually transmitted infections, including chlamydia and trachoma. |
Transformation is one of the processes through which Gram-negative bacteria acquire new genetic material from their surroundings, contributing to their adaptability and resistance. This process, along with conjugation and transduction, allows bacteria to exchange genes, including those for antibiotic resistance. Medically important Gram-negative bacteria that undergo horizontal gene transformation include Helicobacter pylori, Neisseria meningitidis, and Pseudomonas aeruginosa.
Gram-negative bacteria represent a diverse and highly adaptable group of microorganisms that pose significant challenges in both clinical and environmental contexts. Their unique double-membrane structure enhances their resistance to antibiotics and environmental stressors, making them persistent and often dangerous pathogens. Ongoing research into more effective treatments, including developing microbiome-targeted interventions (MBTIs) and alternative therapies, is critical for managing infections caused by these bacteria.
The key difference lies in the structure of their cell walls. Gram-negative bacteria have a thin peptidoglycan layer and an outer membrane with LPS, while Gram-positive bacteria have a thicker peptidoglycan layer and lack an outer membrane. These structural differences affect their susceptibility to antibiotics and staining properties in the Gram stain test.
Gram-negative bacteria, such as Pseudomonas aeruginosa and Acinetobacter baumannii, are major causes of hospital-acquired infections. These bacteria can thrive in healthcare settings and are often resistant to multiple antibiotics, making infections difficult to treat.
Yes, Gram-negative bacteria are widely found in natural environments, including soil, water, and plants. Some species are harmless or even beneficial in certain ecosystems, while others can become pathogenic under specific conditions.
While there are vaccines for some Gram-negative bacteria, such as Neisseria meningitidis (which causes meningitis), vaccines for other Gram-negative pathogens like Pseudomonas aeruginosa or Klebsiella pneumoniae are still under development.
2024-09-24 12:28:53
Gram-Negative Bacteria majorpublished
Microbiome Targeted Interventions (MBTIs) are cutting-edge treatments that utilize information from Microbiome Signatures to modulate the microbiome, revolutionizing medicine with unparalleled precision and impact.
Silhavy TJ, Kahne D, Walker S.
The bacterial cell envelope.https://doi.org/10.1101/cshperspect.a000414