2025-01-14 13:43:44
Bradford Hill Criteria majorpublished
Did you know?
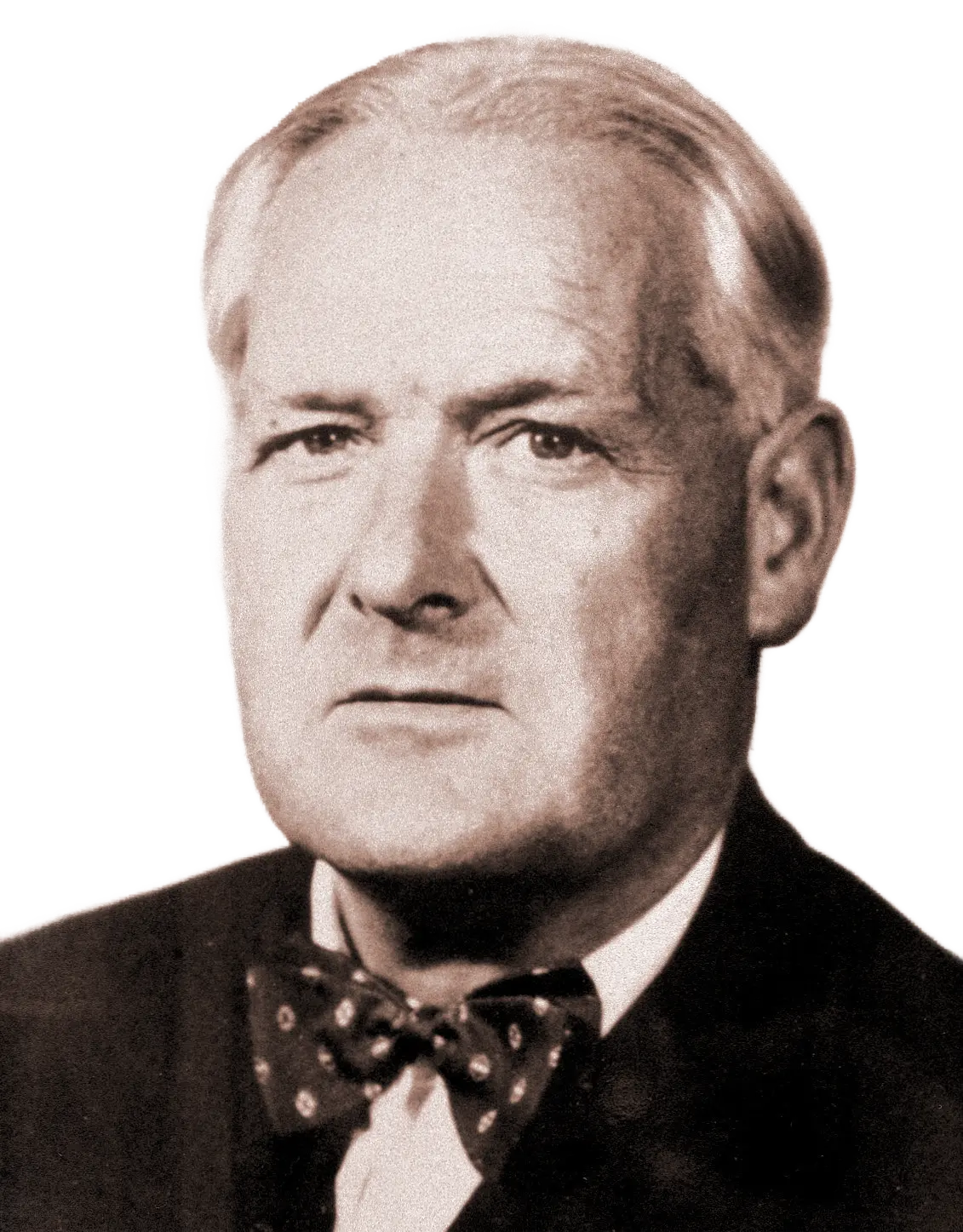
Sir Austin Bradford Hill was not only responsible for pioneering the Bradford Hill Criteria but also played a critical role in establishing the first randomized controlled trial (RCT) in medical research. In 1948, he and Richard Doll proved streptomycin’s effectiveness against tuberculosis, revolutionizing clinical trials. Despite this, Hill later argued RCTs weren’t always needed to prove causation—leading to his landmark criteria in epidemiology.
The Bradford Hill Criteria emphasized a holistic assessment of evidence to determine causality rather than requiring rigid experimental proof.
Karen Pendergrass is a microbiome researcher specializing in microbiome-targeted interventions (MBTIs). She systematically analyzes scientific literature to identify microbial patterns, develop hypotheses, and validate interventions. As the founder of the Microbiome Signatures Database, she bridges microbiome research with clinical practice. In 2012, based on her own investigative research, she became the first documented case of FMT for Celiac Disease—four years before the first published case study.
Microbiome Signatures identifies and validates condition-specific microbiome shifts and interventions to accelerate clinical translation. Our multidisciplinary team supports clinicians, researchers, and innovators in turning microbiome science into actionable medicine.
Karen Pendergrass is a microbiome researcher specializing in microbiome-targeted interventions (MBTIs). She systematically analyzes scientific literature to identify microbial patterns, develop hypotheses, and validate interventions. As the founder of the Microbiome Signatures Database, she bridges microbiome research with clinical practice. In 2012, based on her own investigative research, she became the first documented case of FMT for Celiac Disease—four years before the first published case study.
The Bradford Hill Criteria were introduced by Sir Austin Bradford Hill, a British epidemiologist and statistician, in a 1965 lecture titled “The Environment and Disease: Association or Causation?” The framework was developed to guide researchers in determining whether observed associations between a potential exposure and a disease could be interpreted as causal. This was particularly critical in fields like public health, where randomized controlled trials (RCTs) were often unfeasible, unethical, or impractical. Bradford Hill proposed nine principles that could be used as a logical framework for assessing causality: strength of association, consistency, specificity, temporality, biological gradient (dose-response), plausibility, coherence, experiment, and analogy.
Despite its revolutionary impact on public health, the Bradford Hill Criteria have been largely overlooked in fields like microbiome research, where RCTs are impractical, but action is nonetheless urgently needed. If we continue waiting for decades of traditional epidemiological validation, we risk delaying life-saving microbiome-targeted interventions. Here we posit that modernizing Bradford Hill’s framework is essential for unlocking the next public health breakthrough.
Over the decades, advances in causal inference have refined the Bradford Hill Criteria, integrating statistical models, computational tools, and alternative frameworks such as Directed Acyclic Graphs (DAGs), Sufficient-Component Cause Models (SCC models), and GRADE (Grading of Recommendations, Assessment, Development, and Evaluation). These refinements address limitations in traditional causal assessment, particularly in observational data settings where confounding and bias must be rigorously accounted for. Modern approaches emphasize the distinction between associational causality (where two factors correlate) and manipulative causality (where altering an exposure leads to predictable changes in an outcome). This shift is crucial for policy-driven research, including microbiome studies, where direct experimental interventions are often impractical. This is not just an academic debate; it is a paradigm shift. The future of microbiome research depends on breaking free from outdated epidemiological models and embracing structured, computationally-driven causation frameworks.
The Bradford Hill Criteria were pivotal in the mid-20th century during debates about the health risks of cigarette smoking. By the 1940s and 1950s, epidemiological studies, such as those conducted by Richard Doll and Bradford Hill himself, revealed a strong correlation between smoking and lung cancer. However, skepticism lingered because smoking was a pervasive societal habit, and proving causation through RCTs was impossible. Nonetheless, using the Bradford Hill Criteria, researchers systematically evaluated the evidence. Ultimately, the comprehensive application of the Bradford Hill Criteria established causation, leading to widespread acceptance of smoking as the primary cause of lung cancer:
Strength: Smokers were found to have much higher rates of lung cancer than non-smokers.
Consistency: Similar findings were replicated across numerous studies, populations, and contexts.
Temporality: Smoking clearly preceded the development of lung cancer in case studies and cohort analyses.
Biological gradient: Heavy smokers had a greater risk of lung cancer than light or occasional smokers.
Plausibility: Laboratory studies demonstrated that tobacco smoke contains carcinogens capable of causing cellular mutations.
If we had waited for RCTs to confirm smoking’s role in lung cancer, we would have lost decades of progress. The same mistake is being repeated today in microbiome research.
The Bradford Hill Criteria underscore the importance of addressing public health crises when waiting for perfect evidence is impractical or unethical. In contexts where RCTs are too costly, time-consuming, or logistically infeasible, these criteria provide a structured approach to evaluate evidence and make informed decisions.
In microbiome research, traditional epidemiological methods often fall short due to:
The complexity of microbial ecosystems, where multiple interactions occur simultaneously.
The need for longitudinal studies to establish causation.
The immense cost and time required for large-scale RCTs.
The 30-50 year translational gap projected for microbiome research to reach clinical practice.
Given the urgency of conditions linked to the microbiome—such as endometriosis,Parkinson’s disease, and metabolic disorders—waiting decades for definitive evidence is unacceptable when public health is at stake.
Modern causal inference approaches provide new tools to validate microbiome-targeted interventions (MBTIs). These approaches align with our MBTI Validation Criteria, which incorporate microbiome signature alignment, clinical efficacy, and dual validation:
Directed Acyclic Graphs (DAGs): These allow researchers to model complex relationships between microbiota and disease outcomes while controlling for confounding variables.
Sufficient-Component Cause Models (SCC Models): These models emphasize multi-factorial causation, which aligns well with microbiome research where multiple microbes may contribute to a condition.
Mutual Information and Causal Graphs: These computational techniques improve upon traditional association-based measures by identifying predictive causation, rather than mere correlation.
Dose-Response Refinements: Recent critiques suggest that dose-response relationships can be confounded. In microbiome research, this means looking at the effects of different levels of microbial shifts, rather than simple exposure-outcome trends.
Critics argue that without RCTs, causal claims in microbiome research are weak. However, the same logic was used to delay the recognition of smoking’s health risks. With modern causal inference tools—DAGs, Bayesian networks, and microbiome signatures—we can achieve the same level of confidence without waiting 50 years.
Microbiome research stands at a crossroads. We can either cling to outdated methodologies and wait 30 years for a consensus—or we can apply causal inference tools now to start saving lives. By integrating advanced statistical tools, causal inference methods, and computational models, we can accelerate progress, bridge translational gaps, and improve global health outcomes. The principles of causal inference should evolve, but the core mission remains the same: using structured, logical frameworks to drive actionable change in public health. The choice is ours.
The Bradford Hill Criteria are a set of nine principles developed by Sir Austin Bradford Hill in 1965 to help determine whether an observed association between an exposure and an outcome is causal.
They were designed to assess causation in epidemiological studies, particularly when randomized controlled trials (RCTs) were impractical or unethical.
Yes, but they have been refined with modern causal inference techniques like Directed Acyclic Graphs (DAGs), Bayesian networks, and computational models to address contemporary scientific challenges.
No single criterion can definitively prove causation, but together they provide a structured approach for evaluating causal relationships.
No. Some criteria (like temporality) are more essential than others, and not all need to be met for a strong causal argument.
Temporality (the cause must precede the effect) is often considered the most fundamental.
The specificity criterion is considered weak because many diseases have multiple causes. The analogy criterion is sometimes seen as subjective. The dose-response criterion can be confounded by other variables. And lastly, the criteria cannot fully account for complex, multi-factorial conditions like those in microbiome research.
Traditional epidemiological models struggle with complex interactions, confounding, and observational biases. Modern computational tools like DAGs, Bayesian networks, and machine learning enhance causal inference beyond what the original criteria could address.
RCTs are considered the gold standard for establishing causality, but when RCTs are impractical, the Bradford Hill Criteria provide an alternative logical framework.
They help evaluate whether specific microbial imbalances contribute to diseases, even when RCTs are not feasible.
Waiting decades for RCTs to confirm microbiome-disease relationships delays life-saving interventions. The Bradford Hill framework, modernized with computational tools, enables faster and more actionable conclusions.
Directed Acyclic Graphs (DAGs) for controlling confounding variables
Sufficient-Component Cause Models (SCC Models) to account for multi-factorial causation
Bayesian Networks & Causal Graphs for predictive analysis
Mutual Information Metrics to quantify statistical dependencies
2025-01-14 13:43:44
Bradford Hill Criteria majorpublished
Endometriosis involves ectopic endometrial tissue causing pain and infertility. Validated and Promising Interventions include Hyperbaric Oxygen Therapy (HBOT), Low Nickel Diet, and Metronidazole therapy.